Community-Based Primary Health Care (CBPHC) Common Indicator Project
Overview
The 12 CBPHC Innovation Teams were funded to implement cross-jurisdictional programs in improving access to CBPHC for vulnerable populations and chronic disease prevention and management. The teams are collaborating on a set of common indicators to measure the impact and benefits of this research investment on the provision of primary health care. This unprecedented work is led by a working group co-chaired by Sabrina Wong (University of British Columbia) and Jeannie Haggerty (McGill University) with representation from all 12 teams, the CIHR Institutes of Health Services and Policy Research and Population and Public Health, in collaboration with the Canadian Institute for Health Information (CIHI). The research questions, process, and agreed upon dimensions being measured are all outlined below.
Project Research Questions
- What is the impact of improving community-based primary health care (CBPHC) access for vulnerable populations and of innovations in chronic disease prevention and management on CBPHC outputs (access to care, acceptability, comprehensiveness, coordination) and outcomes (effectiveness and health equity) across various populations?
- What is the impact of alternative models of chronic disease prevention and management in CBPHC on patient and system outcomes (e.g., health outcomes, cost, access, equity) across all 12 Teams at the program level?
- What are the structures (e.g. governance, financing, etc.) and context that influence the cost, implementation and delivery potential for scale-up and impact of CBPHC models of care across all 12 Teams at a program level?
Note: This work represents a world first in comparative research. As such, a by-product of this work will be documentation and analysis of the underlying methods, theories, or frameworks that can be used to advance the science of comparative research.
Process to date
Following a review of existing primary health care indicators (e.g. CIHI) and the research protocols for each of 12 Teams, the working group identified, through a consensus building process, several dimensions important to primary health care and related constructs (e.g. multimorbidity, demographic characteristics). This group has agreed upon common measures that use publicly available and previously validated data collection instruments (e.g. patient and provider surveys). While not all dimensions will be measured by all teams, 75% coverage for agreed upon dimensions across all teams has been achieved. Data collection using patient and provider/organizational self-report and administrative data is currently underway.
Agreed upon dimensions of primary health care
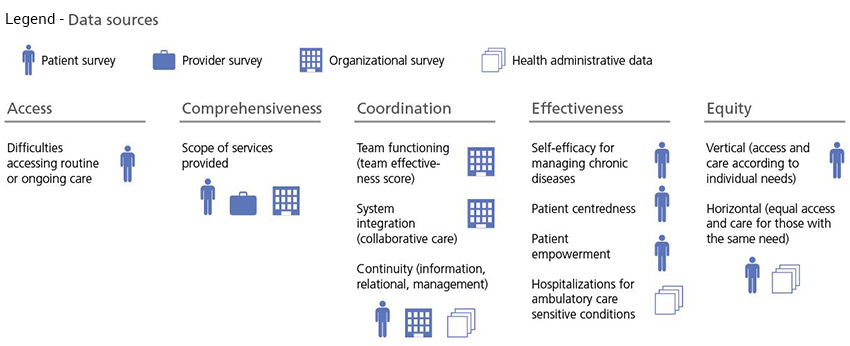
Agreed upon dimensions of primary health care - Long description
Access
- Difficulties accessing routine or ongoing care (measured by patient surveys)
Comprehensiveness
- Scope of services provided (measured by patient surveys, provider surveys, and organizational surveys)
Coordination
- Team functioning - team effectiveness score (measured by organizational surveys)
- System integration - collaborative care (measured by organizational surveys)
- Continuity - information, relational, management (measured by patient surveys, organizational surveys and health administrative data)
Effectiveness
- Self-efficacy for managing chronic diseases (measured by patient surveys)
- Patient centredness (measured by patient surveys)
- Patient empowerment (measured by patient surveys)
- Hospitalizations for ambulatory care sensitive conditions (measured by health administrative data)
Equity
- Vertical – access and care according to individual needs (measured by patient surveys)
- Horizontal – equal access and care for those with the same need (measured by patient surveys and health administrative data)
Patient and health system information
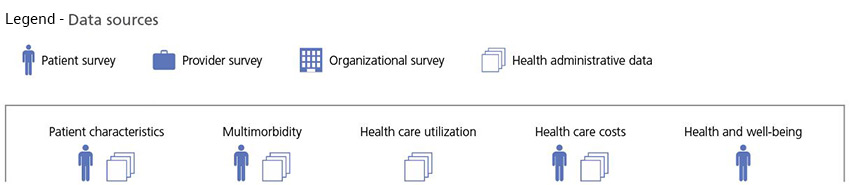
Patient and health system information - Long description
- Patient characteristics (measured by patient surveys and health administrative data)
- Multimorbidity (measured by patient surveys and health administrative data)
- Health care utilization (measured by health administrative data)
- Health care costs (measured by patient surveys and health administrative data)
- Health and well-being (measured by patient surveys)
- Date modified: